HL7 & FHIR Integration Services
Healthcare interoperability services for secure, scalable data exchange across clinical and administrative systems
Business First
Code Next
Let’s talk
- HL7
- FHIR
- CDA
- HL7 integration engine
- Data mapping
- Interface development
- Interface integration
- Interoperability
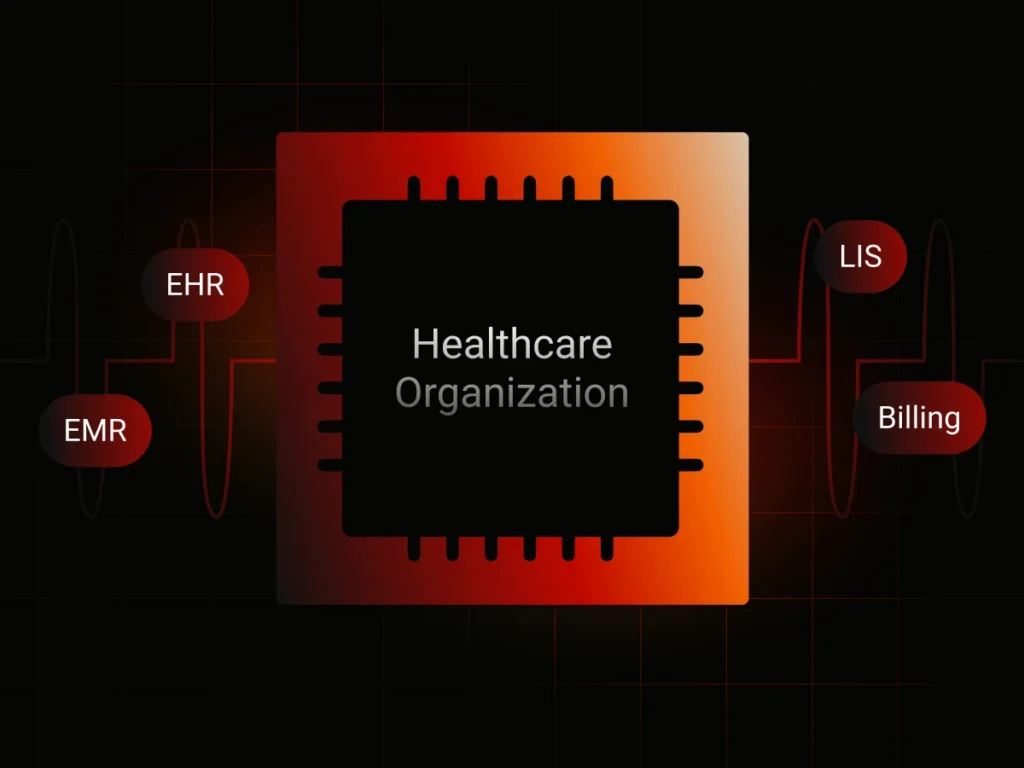
Healthcare Interoperability Challenges
Healthcare interoperability initiatives often stall due to legacy complexity, fragmented data, and poorly governed integrations. HL7 and FHIR standards alone do not guarantee reliable data exchange without a structured integration approach.
Organizations typically face:
- Disconnected EHR, EMR, LIS, and billing systems
- Legacy HL7 interfaces lacking documentation and ownership
- Inconsistent clinical and administrative data across platforms
- High operational and compliance risk during integration changes
- Slow onboarding of new healthcare systems and partners
Our healthcare interoperability services address these challenges through controlled HL7 and FHIR integration delivery.
HL7 & FHIR Integration Services
We deliver end-to-end healthcare data integration services covering both legacy and modern interoperability standards.
Design and implementation of stable HL7 interfaces for real-time and batch healthcare data exchange, including message parsing, transformation, routing, validation, and reconciliation across clinical and administrative systems.
Normalization and transformation of clinical and administrative data between HL7, FHIR, and proprietary formats to ensure consistency, data quality, and operational reliability.
Stabilization and modernization of outdated HL7 integrations through reverse engineering, refactoring, and phased migration toward FHIR-based interoperability architectures without disrupting patient care.
Implementation of FHIR-based interoperability using secure APIs, including HL7-to-FHIR mapping, FHIR resource modeling, SMART on FHIR integrations, and controlled access to clinical data for internal and third-party systems.
Setup, configuration, and optimization of healthcare integration engines to support high message volumes, monitoring, logging, and predictable performance in production environments.
Secure healthcare data exchange with access control, audit logging, traceability, and ongoing production support to meet regulatory and operational requirements.
Discuss your HL7 or FHIR integration scenario
Business First
Code Next
Let’s talk
Common Healthcare Interoperability Use Cases
Business-driven HL7 and FHIR integration scenarios focused on operational continuity, risk reduction, and scalable healthcare data exchange.
EHR and EMR system integration
Secure exchange of patient, encounter, and clinical data across core healthcare systems.
Laboratory and diagnostic data exchange
Integration between LIS, RIS, and clinical platforms using HL7 messaging and FHIR resources.
Healthcare platform interoperability
Connecting digital health products with hospital and provider ecosystems.
Multi-facility data synchronization
Consistent patient and operational data exchange across hospitals, clinics, and care networks.
Legacy healthcare system modernization
Gradual transition from brittle HL7 interfaces to scalable interoperability architectures.
Industry leaders—powered by our expertise
Discover how our healthcare software development company empowers businesses with cutting-edge custom solutions, driving advancements in patient care.
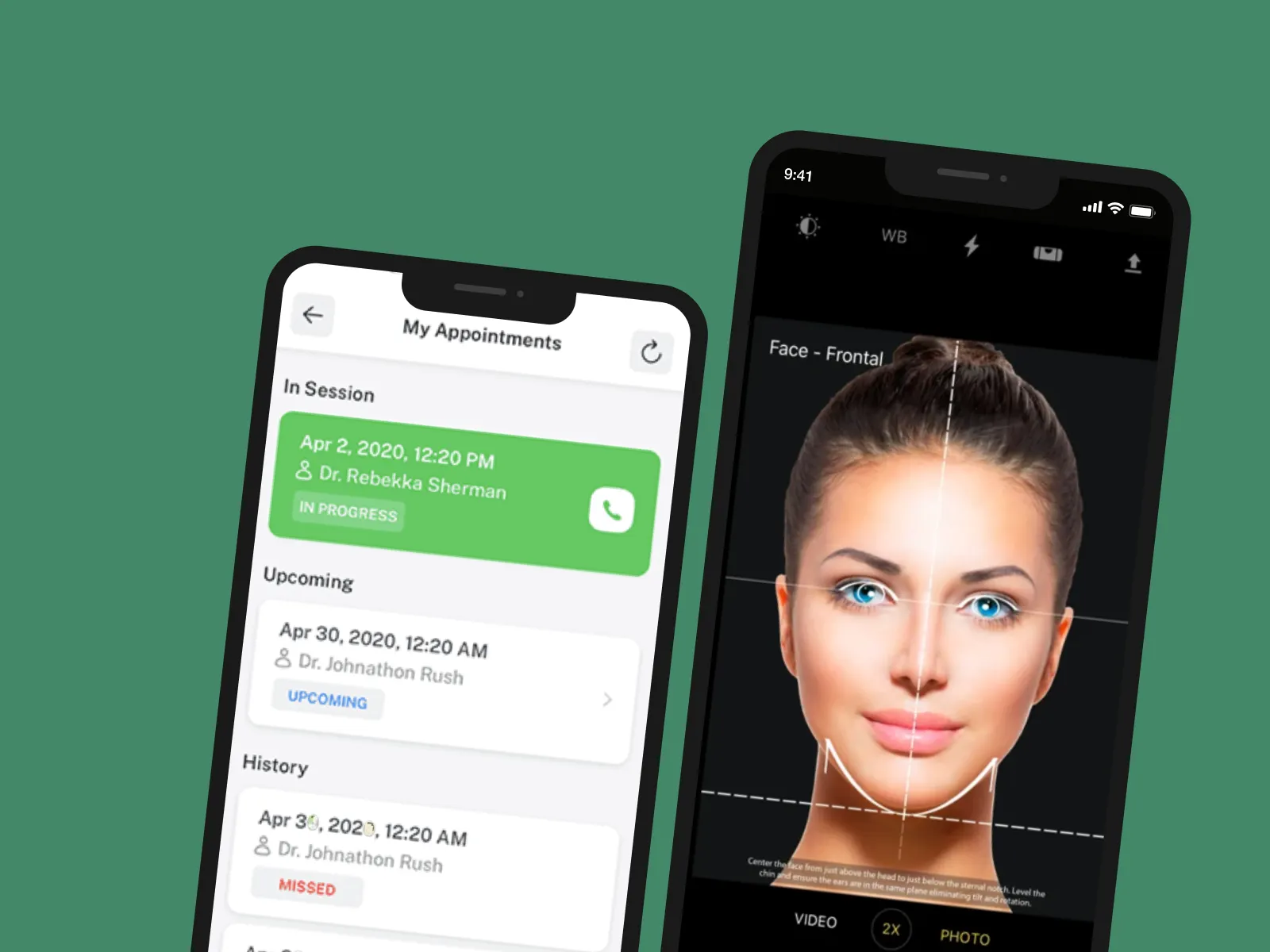
RxPhoto
Medical photography management platform
The solution helps healthcare professionals run the “before-after” analysis. The photography management tool is cloud-based and HIPAA-compliant.
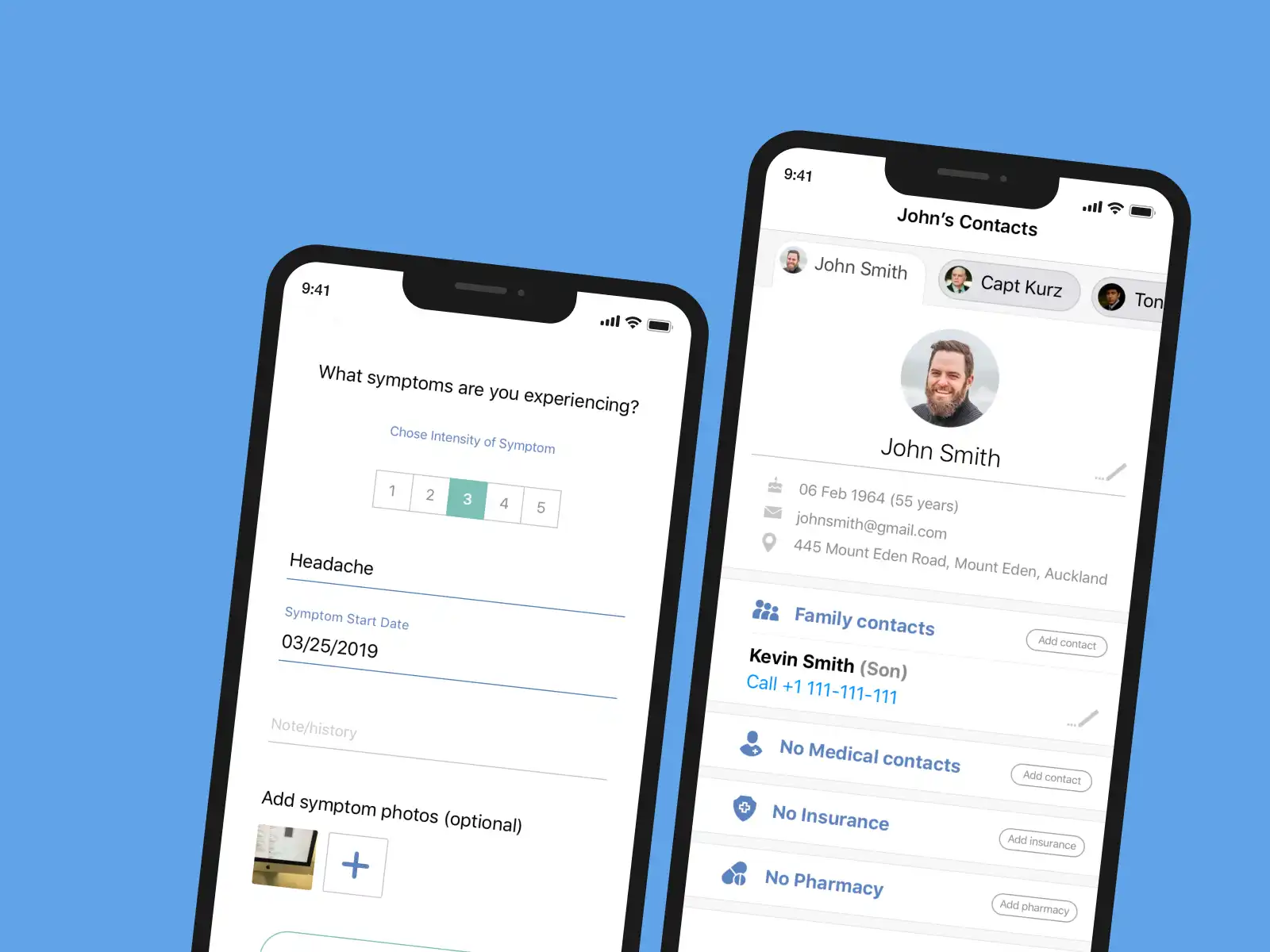
HealthSync
Medical information management platform
The platform is a one-stop solution for medical specialists and caregivers. It helps track symptoms, medications, conditions, and other metrics. Also, it provides the opportunity to book appointments and get health reports.
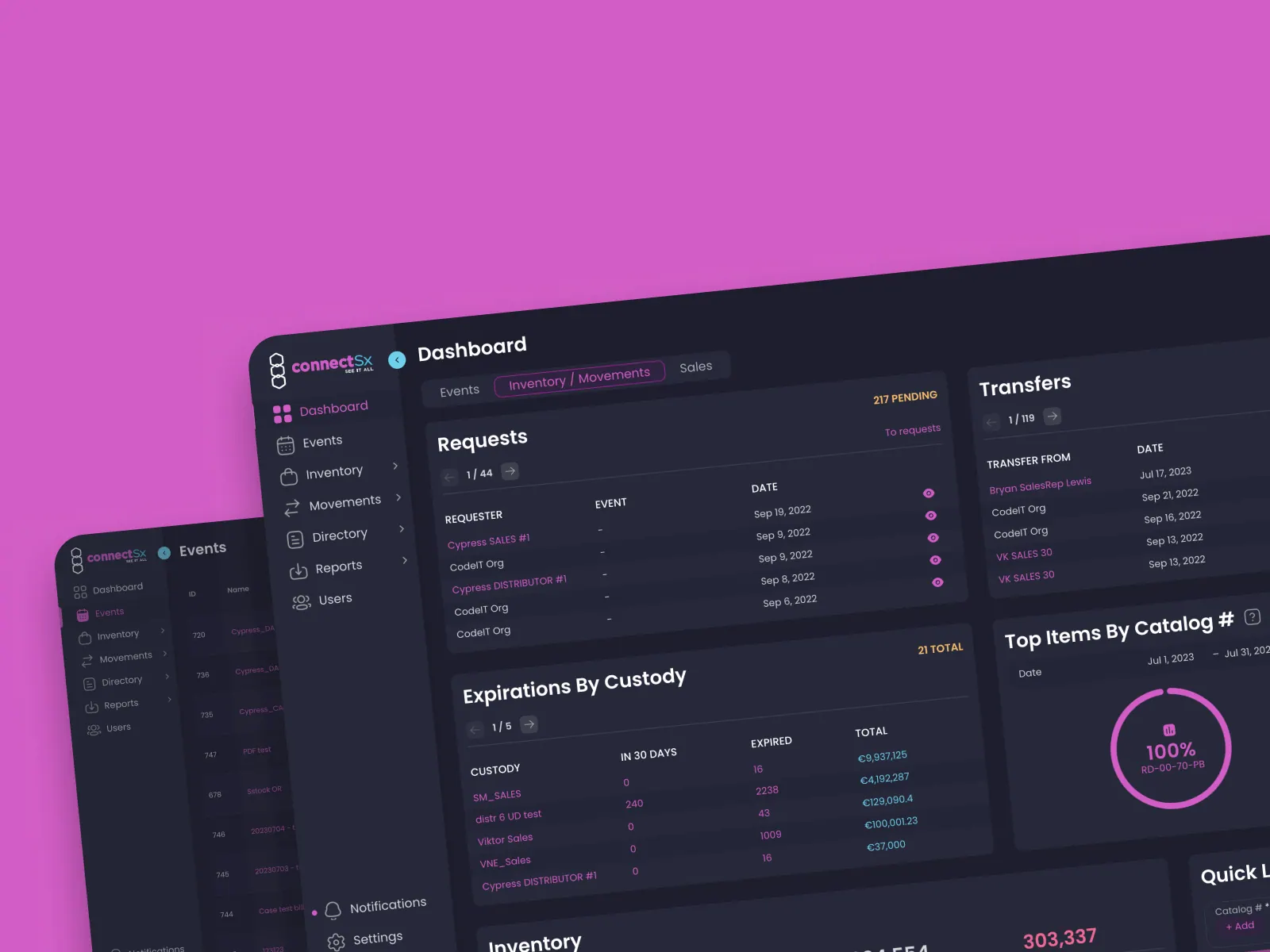
ConnectSx
Medical Inventory Management Apps
The solution comprises one web- and two mobile-based applications. They enable seamless inventory management and monitoring.
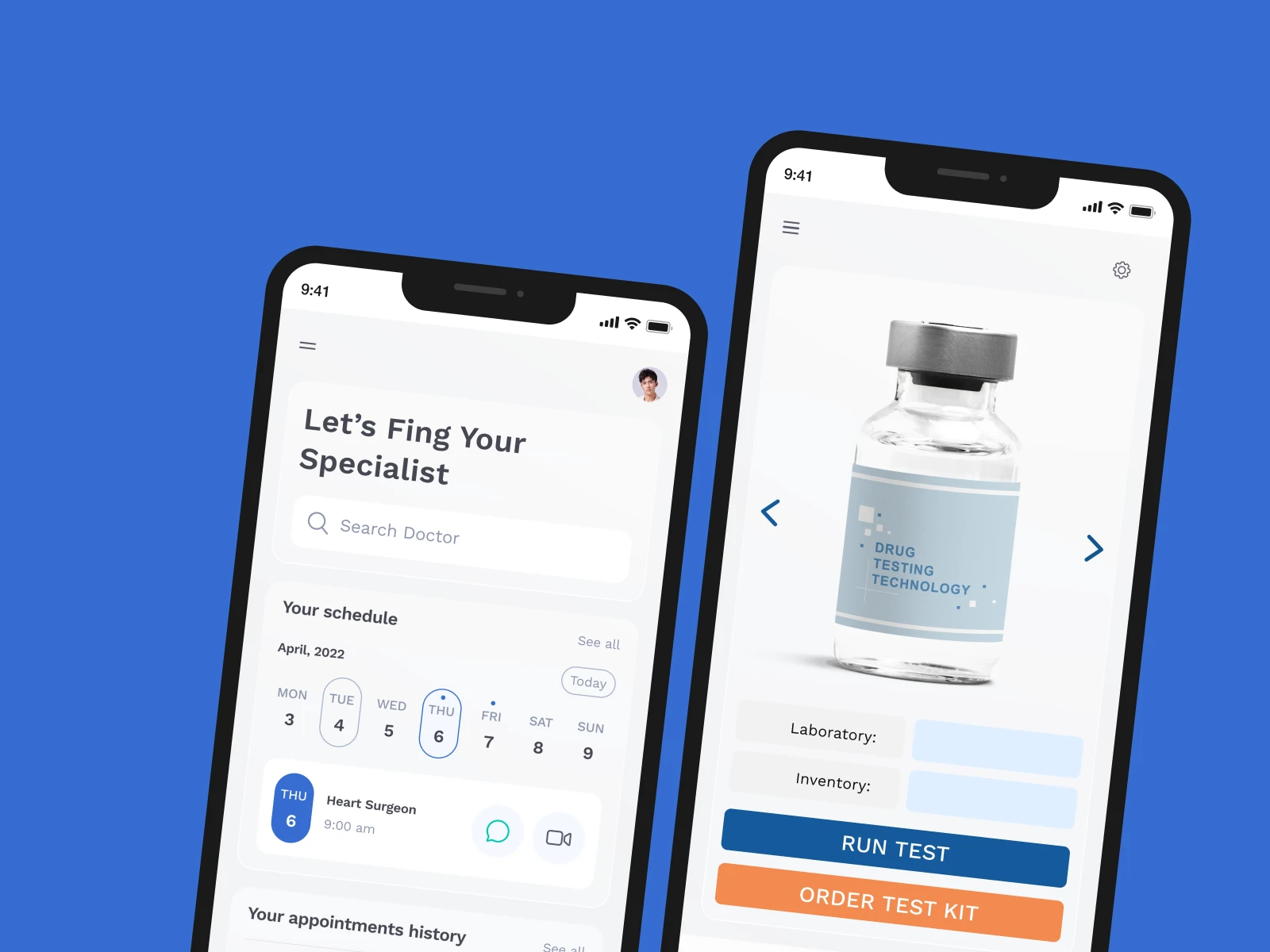
Solution for online medical laboratory
The mobile app streamlines lab analysis and documentation creation.
The custom web application for laboratory equipment testing helps simplify, automate, and improve the quality assurance process of lab instruments.
Software for medical laboratory equipment
- Experiment planning
- Lab analysis integration
- Test result management
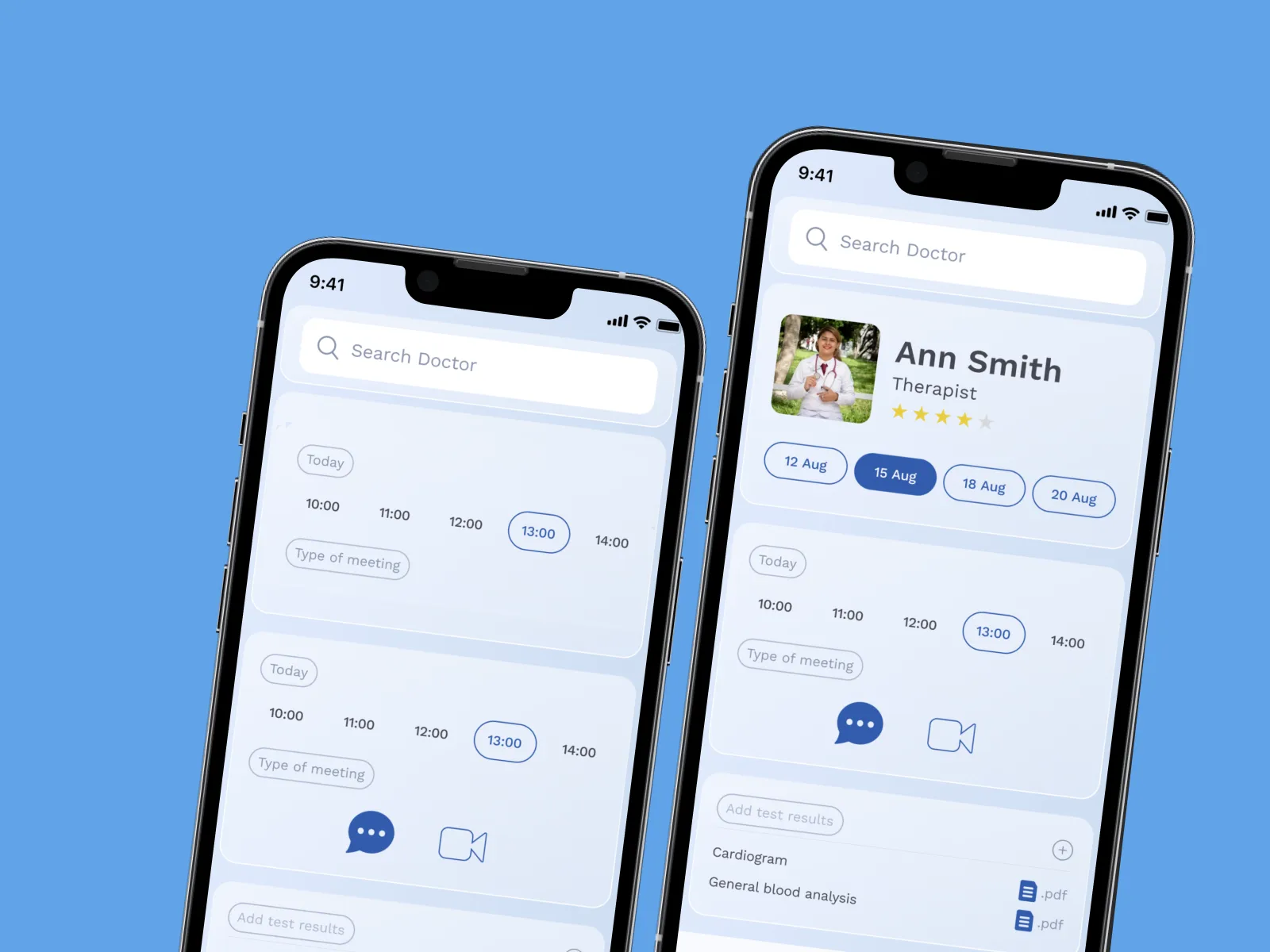
Telemedicine and Doctor Appointment App
The mobile app is integrated with the client’s medical system. It helps patients quickly find the best doctors and book appointments online.
Why Healthcare Teams Choose CodeIT
Healthcare teams choose CodeIT to reduce integration risk, simplify interoperability decisions, and maintain stable, compliant data exchange as their systems evolve.
Clear interoperability strategy, not just implementation
We align HL7 and FHIR integration decisions with business, operational, and clinical goals.

Risk-aware healthcare integration delivery
Integration risks are identified early and managed throughout the lifecycle.

Vendor-neutral integration approach
Our solutions integrate with existing systems rather than forcing platform replacement.
Get your HL7 implementation roadmap
Business First
Code Next
Let’s talk
What to Expect When You Start
Interoperability Discovery
We start with a focused discovery phase to understand how healthcare data currently moves across your systems and where interoperability risks exist. This step establishes a shared understanding between business and technical stakeholders before any integration work begins.
During discovery, we:
- Review existing HL7 and FHIR interfaces and data flows
- Identify connected systems such as EHR, EMR, LIS, billing, and external platforms
- Assess data exchange reliability, ownership, and documentation gaps
- Clarify compliance, security, and operational constraints
The result is a clear, practical view of your current interoperability landscape, including risks, dependencies, and improvement opportunities.
Integration Architecture & Roadmap
Based on discovery findings, we design a healthcare interoperability architecture that supports both current operations and future growth. This step translates integration complexity into a clear, manageable plan.
This phase includes:
- Defining how HL7 and FHIR standards will be applied across systems
- Designing data mapping and transformation strategies
- Identifying legacy components requiring stabilization or modernization
- Creating a phased integration roadmap with dependencies and priorities
You receive a realistic integration plan that reduces uncertainty and supports informed decision-making.

HL7 & FHIR Implementation
With the architecture in place, we move into controlled implementation of HL7 and FHIR integrations. The focus is on building stable, production-ready healthcare data exchange aligned with real workflows.
Implementation typically covers:
- HL7 interface development and customization
- FHIR API implementation and HL7-to-FHIR mapping
- Integration engine configuration and optimization
- Secure data exchange and access control setup
All integrations are built and tested against real-world scenarios to ensure accuracy and operational stability.

Validation & Production Readiness
Before production release, we validate that healthcare interoperability works reliably under operational conditions. This step minimizes disruption and reduces post-launch risk.
Validation activities include:
- Message validation and data consistency checks
- Error handling and recovery testing
- Performance and load verification
- Security, access, and audit readiness review
This ensures HL7 and FHIR integrations are ready for continuous, dependable operation.

Operational Support & Optimization
After go-live, we support and optimize your healthcare interoperability ecosystem to ensure long-term stability and scalability. This phase focuses on sustaining reliable data exchange while reducing internal operational load.
Ongoing support includes:
- Monitoring and incident resolution
- Performance tuning and optimization
- Adaptation to system changes and new integration needs
- Continuous improvement of integration reliability
The result is a maintainable, scalable interoperability environment that evolves with your healthcare systems.

FAQ
The timespan required for completing HL7 integration services varies from weeks to months because of many factors, including:
- The number of systems and message types to implement
- Legacy software limitations
- Technical documentation and a data source map
- Custom requirements
The foremost types of HL7 messages are related to data transfer, submission, appointment scheduling, and more.
- ADT—Admit, discharge, and transfer
- ORM—Order entry
- ORU—Observation result
- MDM—Medical document management
- DFT—Detailed financial transactions
- BAR—-Billing account record
- SIU—Scheduling information unsolicited
- RDE—Pharmacy/treatment encoded order
- RDS—Pharmacy/treatment dispense
- ACK—Acknowledgment message
The final cost depends on the number of HL7 consultants involved and the time devoted to a project. A thorough project analysis is required to estimate the timeline and budget.
CodeIT experts have top-tier industry expertise in building custom digital solutions that comply with HIPAA-compliant integration and other regulatory requirements. The core activities include:
- Data encryption
- Role-based access control
- Activity monitoring and log audit
- Secure API development
- Risk analysis and response plan creation
We build custom point-to-point integrations or API-based connections and develop data transformation and validation tools to connect solutions from diverse vendors seamlessly.
Yes. At CodeIT, we provide after-development support. Also, we process change requests as an additional service.
Yes. We can implement HL7 to FHIR conversion tools to convert HL7 V2 to FHIR automatically.